Ontario supports McMaster COVID-19 research
McMaster University researchers have been awarded funding for five pandemic studies in the first announcement by the Ontario government of COVID-19 Rapid Research Fund projects.
“There’s no reason why a new rapid testing method, vaccine or treatment can’t be found right here in Ontario,” said Premier Doug Ford, in announcing the funding of the first 15 projects.
“Our government is investing in some very promising research proposals, which have the potential to save lives and help us get back to a way of life that is as close to normal as possible.”
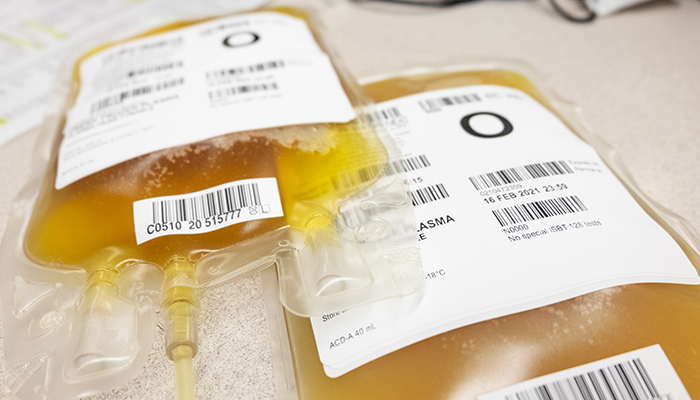
The university’s largest grant, for $1.2 million, is for the major national study led by Donald Arnold, associate professor of medicine, on the use of blood, known as convalescent plasma, from recovered pandemic patients for the treatment of patients fighting the virus. The clinical trial to test effectiveness of the treatment will enrol patients who are 16 or older with COVID-19 who have been admitted to hospital and require supplemental oxygen for the respiratory illness.
The national study, called CONCOR-1, involves more than 60 hospitals and universities across Canada, the Canadian Blood Services, Héma-Québec, along with three hospitals in New York City and the New York Blood Center.
“This is perhaps the largest clinical trial of convalescent plasma for COVID-19 in the world, run out of Ontario,” said Arnold. “The trial is a huge collaborative effort, implemented in record time and carefully designed to evaluate the efficacy of this new therapeutic.”
A related study being led by associate professor of medicine Ishac Nazy was awarded $400,000 to determine whether immunity to COVID-19 is longstanding or if it wanes over time, and to determine how immune-based treatments, either convalescent plasma or future vaccines, work to fight off the virus.
The goal of the research project is to determine the makeup, concentration, strength and viral properties of anti-SARS-CoV-2 antibodies, in order to provide insights into the immune response of individuals infected with COVID-19. Working with Arnold, this research will use samples from recovered patients to test for the antibodies, see how long they last, and determine if they can bind and neutralize the virus.
A third study, with a grant over $15,000, will work to improve COVID-19 detection in children and adults who lack respiratory symptoms, are considered asymptomatic, or are presumed to have “recovered” from past infection, by examining stool samples.
The three co-principal investigators are Nikhil Pai, associate professor of pediatrics; Jeffrey Pernica, associate professor of pediatrics, and Marek Smieja, professor of pathology and molecular medicine.
The team is developing a novel diagnostic test to help detect COVID-19 from stool. They are looking to expand COVID-19 testing options across Canada and to better identify patients who carry a high risk of community transmission than traditional respiratory testing alone.
Co-principal investigators Audrey Lim and Anne Klassen, both associate professors of pediatrics, will use a $65,000 grant to lead the fourth research study looking at how complex pediatric patients fare with the move to virtual clinic settings from hospital visits.
“COVID-19 is placing strain on families of children with medical complexity, fragility and technology dependency,” Lim said.
“Many of these children are dependent on life sustaining technology such as tracheostomy, home mechanical ventilation or feeding tubes. Although accounting for less than one percent of all children in Ontario, this group is at increased risk of multiple and prolonged hospitalizations and poorer health outcomes.”
She added that the children with medical complexity are usually seen at hospital, but with the pandemic, visits are now done through virtual means. Her study will also address the parent’s satisfaction with the virtual complex care clinic healthcare team and may advance the ways virtual health visits are done.
In addition, through St. Joseph’s Healthcare Hamilton (SJHH), professor Marek Smieja is leading a fifth study, worth $700,000, to increase Ontario’s COVID-19 testing capacity. It will deploy robotic liquid handling technology, specimen pooling, and efficient sample preparation, while reducing biological risk and ensuring reliable results.
The project will bring together the disease diagnostics and development group of SJHH with the Hamilton Regional Laboratory Medicine Program and other clinical laboratories across the province to quickly develop, validate, and deliver high-throughput, COVID-19 testing, with the goal of testing up to 6,000 samples per lab daily.
“We salute the Ontario government on their investment and confidence in our researchers,” said Karen Mossman, acting vice-president, research for McMaster.
“Timing is critical as we all work to fight the effects of COVID-19, and these funds will escalate the work of our researchers who are designing therapeutics, determining treatments, and assisting families to adjust to the realities of virtual clinics.”
2020, Funding